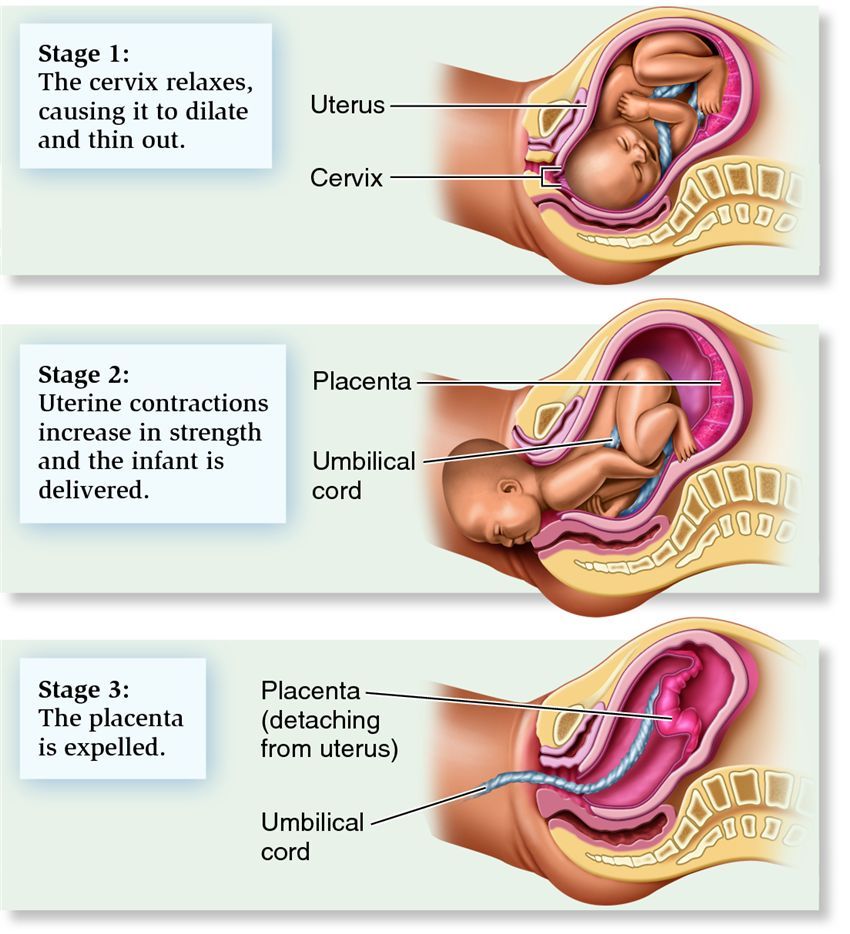
During the 1st stage of labour, contractions make your cervix gradually open (dilate). This is usually the longest stage of labour.
At the start of labour, your cervix starts to soften so it can open. This is called the latent phase and you may feel irregular contractions. It can take many hours, or even days, before you're in established labour.
Established labour is when your cervix has dilated to about 4cm and regular contractions are opening your cervix.
During the latent phase, it's a good idea to have something to eat and drink because you'll need energy for when labour is established.
If your labour starts at night, try to stay comfortable and relaxed. Sleep if you can.
If your labour starts during the day, stay upright and gently active. This helps your baby move down into your pelvis and helps your cervix to dilate.
Breathing exercises, massage and having a warm bath or shower may help ease pain during this early stage of labour.
When to contact a midwife
Contact your midwifery team if:
- your contractions are regular and you're having about 3 in every 10-minute period
- your waters break
- your contractions are very strong and you feel you need pain relief
- you're worried about anything
If you go into hospital or your midwifery unit before your labour has become established, they may suggest you go home again for a while.
Once labour is established, your midwife will check on you from time to time to see how you're progressing and offer you support, including pain relief if you need it.
You can either walk around or get into a position that feels comfortable to labour in.
Your midwife will offer you regular vaginal examinations to see how your labour is progressing. If you do not want to have these, you do not have to – your midwife can discuss with you why she's offering them.
Your cervix needs to open about 10cm for your baby to pass through it. This is what's called being fully dilated.
In a 1st labour, the time from the start of established labour to being fully dilated is usually 8 to 12 hours. It's often quicker (around 5 hours), in a 2nd or 3rd pregnancy.
When you reach the end of the 1st stage of labour, you may feel an urge to push.
Monitoring your baby in labour
Your midwife will monitor you and your baby during labour to make sure you're both coping well.
This will include using a small handheld device to listen to your baby's heart every 15 minutes. You'll be free to move around as much as you want.
Your midwife may suggest electronic monitoring if there are any concerns about you or your baby, or if you choose to have an epidural.
Electronic monitoring involves strapping 2 pads to your bump. One pad is used to monitor your contractions and the other is used to monitor your baby's heartbeat. These pads are attached to a monitor that shows your baby's heartbeat and your contractions
Sometimes a clip called a foetal heart monitor can be attached to the baby's head instead. This can give a more accurate measurement of your baby's heartbeat.
You can ask to be monitored electronically even if there are no concerns. Having electronic monitoring can sometimes restrict how much you can move around.
If you have electronic monitoring with pads on your bump because there are concerns about your baby's heartbeat, you can take the monitor off if your baby's heartbeat is shown to be normal.
A foetal scalp monitor will usually only be removed just as your baby is born, not before.
Speeding up labour
Labour can sometimes be slower than expected. This can happen if your contractions are not coming often enough, are not strong enough, or if your baby is in an awkward position.
If this is the case, your doctor or midwife may talk to you about 2 ways to speed up your labour: breaking your waters or an oxytocin drip.
Breaking your waters
Breaking the membrane that contains the fluid around your baby (your waters) is often enough to make contractions stronger and more regular. This is also known as artificial rupture of the membranes (ARM).
Your midwife or doctor can do this by making a small break in the membrane during a vaginal examination. This may make your contractions feel stronger and more painful, so your midwife will talk to you about pain relief.
Oxytocin drip
If breaking your waters does not work, your doctor or midwife may suggest using a drug called oxytocin (also known as syntocinon) to make your contractions stronger. This is given through a drip that goes into a vein, usually in your wrist or arm.
Oxytocin can make your contractions stronger and more regular and can start to work quite quickly, so your midwife will talk to you about your options for pain relief.
You will also need electronic monitoring to check your baby is coping with the contractions, as well as regular vaginal examinations to check the drip is working.