Pain in your calf, thigh, groin or when you breathe (DVT or PE)
What is Venous Thrombo-embolism (VTE)
Blood usually flows smoothly through all blood vessels. Occasionally, however, blood can form thrombosis or clots in the big veins. These blood clots can also be called venous thrombo-embolisms (VTE). This is a collective term used to describe both Deep Vein Thrombosis (DVT) and Pulmonary Embolism (PE).
A reduction in blood flow combined with an increased clotting tendency can result in a clot in the leg occurring during pregnancy.
This reduction in blood flow is apparent from 16 weeks of pregnancy and becomes slower as your body prepares for birth. It doesn’t return to normal until six weeks after birth. It is this reduction in blood flow which causes many women to experience swelling in their ankles during pregnancy. During the birth process pressure on the veins in the pelvis can cause minor damage to occur, leading to an increased risk of blood clots for up to six weeks after birth.
On average, one to two women in every 1000 will develop a venous thrombosis during pregnancy or just after delivery. However, the majority of these clots can be both prevented and treated.
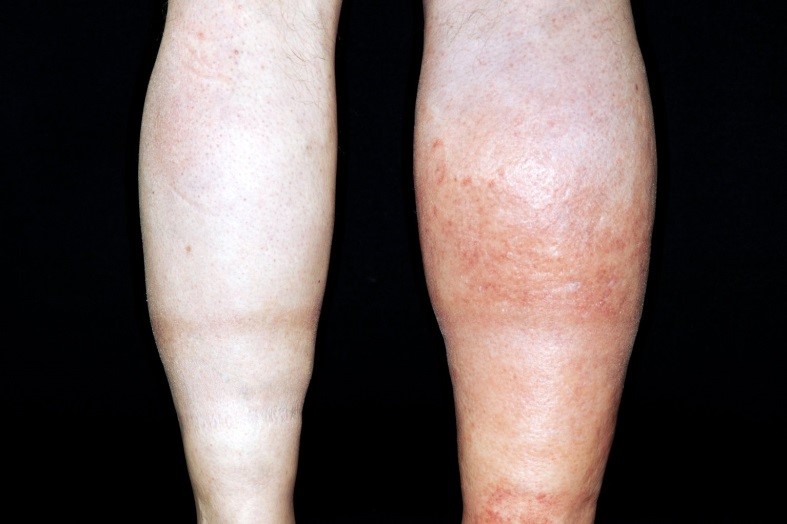
Deep Vein Thrombosis (DVT)
This occurs when a thrombus (blood clot) forms in a deep vein, usually within the leg or pelvis. This results in a reduction in the ow of blood through the vein and may cause it to become blocked.
Symptoms of a venous thrombo-embolism in pregnancy
Symptoms of DVT
• Pain in the calf or thigh associated with swelling of the limb – this may be worse when the foot is bending upwards towards the knee
• Heat or redness particularly in the back of the leg, below the knee
• Difficulty in weight bearing
• DVT usually affects one leg
- During pregnancy, swelling and discomfort in both legs is common and does not always indicate a problem. Always ask your doctor or midwife if you are worried.
- DVT may result in lifelong painful leg swelling, varicose veins and leg ulcers
Picture of a DVT below – typically only affecting one leg and causing it to be larger and red.
Pulmonary Embolism (PE)
Occasionally, part of the DVT breaks off and travels to the lungs. This is known as a pulmonary embolism or PE.
Symptoms of PE:
• Difficulty in breathing or shortness of breath
• Coughing up blood-stained sputum
• Chest pain that is often worse when breathing in
• Can cause collapse in severe cases and may prove to be fatal.
Risks associated with Pregnancy
Pregnant women are ten times more likely to develop venous thombosis than women who are the same age and not pregnant. This is due to the many changes occurring within your body during pregnancy. These changes allow your baby to grow and prepare your body for birth. However, being pregnant:
• makes your blood more likely to clot in order to reduce the risk of heavy bleeding when you give birth.
• slows the speed with which blood flows from your legs back to your heart. This is due to the effect of pregnancy hormones on the veins and also because your womb increases in size as your baby grows.
The symptoms of a PE can sometimes be accompanied by those of a DVT. Seek help immediately if you experience any of the above. If they are persistant please dial 999.
This is a serious condition requiring urgent investigation and treatment.
Risk factors
You are more at risk of developing a VTE during pregnancy if you have any of the following pre-existing risk factors or develop further risk factors during pregnancy:
Pre-existing Risk Factors
• A previous VTE
• A family history of VTE (in parents, or brothers and sisters under the age of 60)
• Significant medical conditions such as:
- thrombophilia
- heart or respiratory disease
- active cancer or cancer treatment
- paraplegia (with significant immobility)
• You are over 35 years of age
• You are overweight (you have a body mass index over 30 at booking)
• Significant varicose veins
• You smoke
• You have had three or more children
Risk Factors developed during pregnancy or during/after birth
• Dehydration and/or hyperemesis (not drinking enough or excessive vomiting)
• You have had assisted reproductive treatment or ovarian hyperstimulation
syndrome and are less than 20 weeks pregnant.
• Immobility for long periods of time. It is important to consider this risk if you:
- are bedbound for three or more days
- have pelvic girdle pain affecting your mobility
– have an epidural
- plan long distance travel exceeding four hours
• Pre-eclampsia
• You have had surgery during this pregnancy (including caesarean section)
• Excessive blood loss or blood transfusion
Prevention
There are a number of steps you can take to reduce your risk of developing VTE. These include:
• Cutting down or stopping smoking
• Maintaining a healthy weight during pregnancy
• Remaining mobile, both during pregnancy and after the birth of your baby.
• Simple leg exercises – Point your toes down and bend the foot up at regular intervals as this helps to pump blood back to the heart. Do this at least ten times an hour during the daytime, particularly when you are inactive for long periods of time.
• Avoiding dehydration – The World Health Organisation recommends a daily intake of three litres of water especially if the weather is warm or you are exercising.
• Multiple pregnancy (twins or more)
How to increase your daily intake of water
• Have a drink of water when you get up in the morning and just before going to sleep (four or five mouthfuls)
• Drink a glass of water instead of decaffeinated tea or coffee
• Every time you go to the toilet drink eight mouthfuls of water to replace the lost fluid
• Never get thirsty.
• Improve your fluid intake by eating watery fruit and vegetables, such as watermelon and cucumber, and include soups and smoothies in your diet.
• Avoid caffeinated drinks and high sugar drinks as these can actually worsen dehydration.
Individual Risk Assessment
You should have your individual risk assessed at your booking appointment, if you are admitted to hospital during your pregnancy, when you go into labour and again immediately after delivery.
Further Preventative Measures
Depending upon your risk of developing VTE you may also be advised to take additional preventative measures. These include:
Anti-embolism stockings
If necessary you will be measured and fitted with knee-length anti-embolism stockings. These work by reducing damage to the leg veins, which distend when you are not mobile. Small tears to these veins cause activation of the clotting mechanism. They also help return blood to the heart.
You should be shown how to wear them and given a factsheet entitled ‘Anti-embolism stockings’ which will explain how to wear them and care for them appropriately. The stockings should be worn day and night if you are in hospital, but can be removed for up to half an hour to wash or have a shower. At home, you should wear them for a minimum of seven days or until you return to your usual level of mobility.
Compression devices
These are inflatable sleeves, which are fitted around the foot or calf whilst you are immobile. They in ate at regular intervals and increase the flow of blood back to the heart.
Medication
The group of drugs used to prevent and treat blood clots are called anticoagulants. During pregnancy you may be given anticoagulants as an injection called low-molecular-weight-heparin (LMWH). This cannot cross the placenta to the baby and is therefore safe to take whilst you are pregnant and breastfeeding.
LWMH will usually only be administered whilst you are in hospital, but if you require injections at home please ensure that a midwife has shown you how to administer this medication and given you a sharps bin to facilitate safe disposal of needles used.
You may notice it takes longer for your blood to clot and you may bruise or bleed more easily. It is important that you tell your doctor or midwife if you experience any long or excessive bleeding, or unexplained bruising.
It is important to continue and finish any course of treatment that you have been given. If you have concerns about the possible side effects of your medication, please discuss them with your midwife or GP as soon as possible.
The length of time you will be advised to administer LMWH depends upon your risk factors and whether your situation changes. However, it is important to discuss the implications of your medication and what you should do when labour starts or if you are having a planned caesarean section, with your obstetrician or midwife at your 36 week antenatal appointment.
You should also ensure the ‘labour ward’ are aware of the frequency and dosage of heparin you are taking if you think you are in labour or have any other cause for concern.
If you have any further questions about the risks of venous thromboembolism and how to prevent blood clots from occurring please speak to your midwife or doctor who will be able to discuss them in greater detail.
If you experience any of the symptoms of VTE at home seek URGENT medical advice from your Midwife, GP, 111, 999 or nearest emergency department.
Sources of further information:
If you have any of the following:
- you have difficulty in breathing or shortness of breath
- you are coughing up blood-stained sputum (spit)
- you have chest pain that is often worse when breathing in
- collapsed of unrousable - the person you are concerned about will not easily wake up
You need urgent help.
Go to the nearest Hospital Emergency (A&E) Department or phone 999
If you have any of the following:
- you have pain in the calf or thigh associated with swelling of the limb - this may be worse when the foot is bending upwards towards the knee
- you have heat or redness particularly in the back of the leg, below the knee
- you have difficulty in weight bearing
- only one leg is affected by these symptoms
- you have pain the groin where your leg meets your pelvis
You need to contact a doctor or midwife today.
Please ring your community midwife, GP surgery or call NHS 111 - dial 111
You do not have the symptoms above.
Self care
Continue providing your care at home. If you are still concerne, call NHS 111 – dial 111